Podcast: Play in new window | Download
- Common during the first year of life as well as during puberty
- Presents with nausea/vomiting, abdominal pain, and/or testicular pain
- ALWAYS examine a child for signs of torsion who presents with abdominal pain (especially lower abdominal pain)
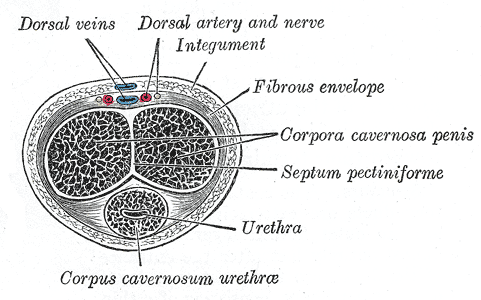
- Look for tenderness, firmness, high riding testicle or testicle with unequal lie, swelling, and the absence of a cremasteric reflex
- Consult Urology IMMEDIATELY if you have high suspicion, otherwise proceed to ultrasound
- Ultrasound is only 85% sensitive, so clinical gestalt can trump even a negative US
- Attempt manual detorsion if there will be a significant delay to surgery